(512) 377-1744
Introduction
- Quality — 30%
- Cost — 30%
- Promoting interoperability — 25%
- Improvement activities — 15%

Eligibility and Participation Requirements
- Bill more than $90,000 in Medicare Part B charges
- Provide care for 200 or more part B patients
- Submit more than 200 part B covered professional services
Key Requirements for 2025
For 2025, all providers should meet following requirements to avoid penalties:
- Report at least 6 quality measures and one of them should be an outcome measure. Otherwise, a high priority measure can be substituted.
- Ensure 75% data completeness for all eligible patients across all payers. The purpose is to make reporting more representative of the facility’s actual performance.
- Score 75 points across all categories to avoid penalties
Quality Measures Updates for 2025
To make the quality measure more reliable and meaningful, CMS has once again refreshed it with following terms:
- 7 new quality measures have been added that any provider can report using traditional MIPS.
- 10 measures have been eliminated as they were either topped out or overlapped with other measures.
- 66 measures have been updated so far with changes to scoring rules, or patient populations.
- Scoring floors policy has been implemented which means you can still earn 5-7 points when reporting for new or revised measures, even before performance benchmarks are set.
- Flat benchmarking will now be used for some topped-outt measures.
CMS wants to prevent minor score differences from making reporting unfair.
- CMS has also added 6 new measures to MIPS Value Pathways (MVPs) across specialties including ophthalmology, gastroenterology, pulmonology, surgical care and urology.

Quality scoring and Benchmarks Updates
Every quality measure you report can earn between 0-10 points. The exact score depends on how much you perform compared to historical benchmarks. Quality is 30% of total score but for small practices, it may count more than 30% if weight of other categories is reduced. Topped-out measures will be capped at fewer points to keep scoring fair. You can be eligible for bonus points if you report more than the required outcome or high priority measures or submit data through end-to-end electronic reporting.
Performance Timeline
Providers will collect quality data throughout the year starting from January 1st through December 31st, 2025. After the year ends, the submission window starts from January 2nd to March 31st, 2026 where practices are expected to submit their data.
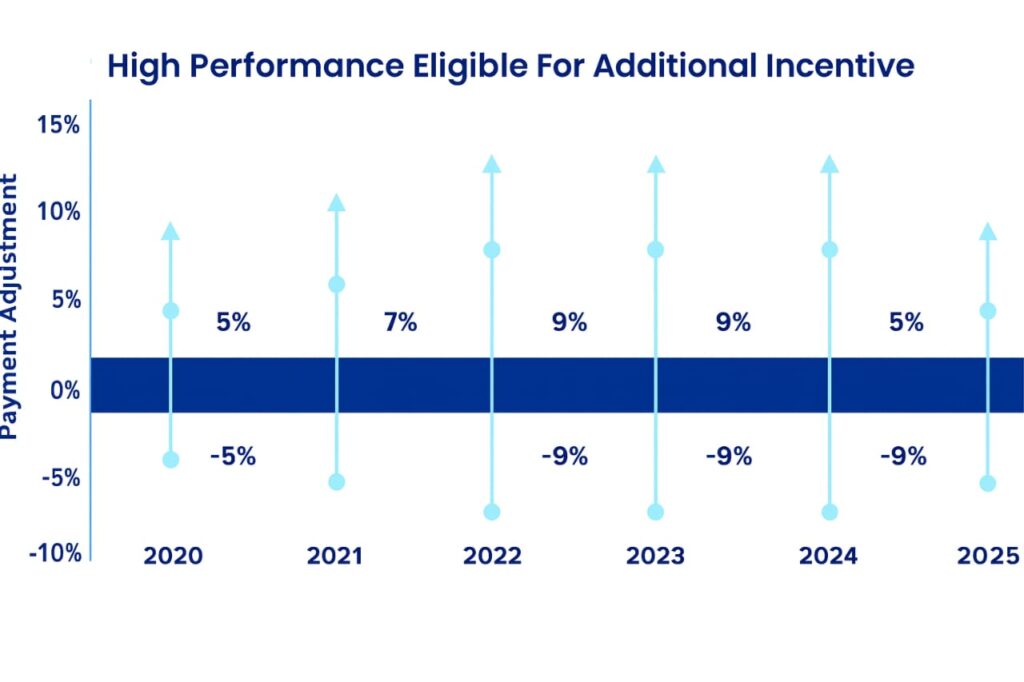
Payment Adjustments
If a provider or group doesn’t submit quality data timely, CMS will apply a maximum penalty of 9% to their Medicare B reimbursements in 2027. Strong quality reporting improves final MIPS scores which can lead to positive adjustments to the final payment. Since the quality category weighs 30% of total score, it makes a difference between penalties and bonuses especially for small practices.
Specialists:
For 2025, CMS has updated more MVPs to make it easier for specialists to only report those measures that apply to their field. This significantly reduces reporting burden and even increases fairness to the process.
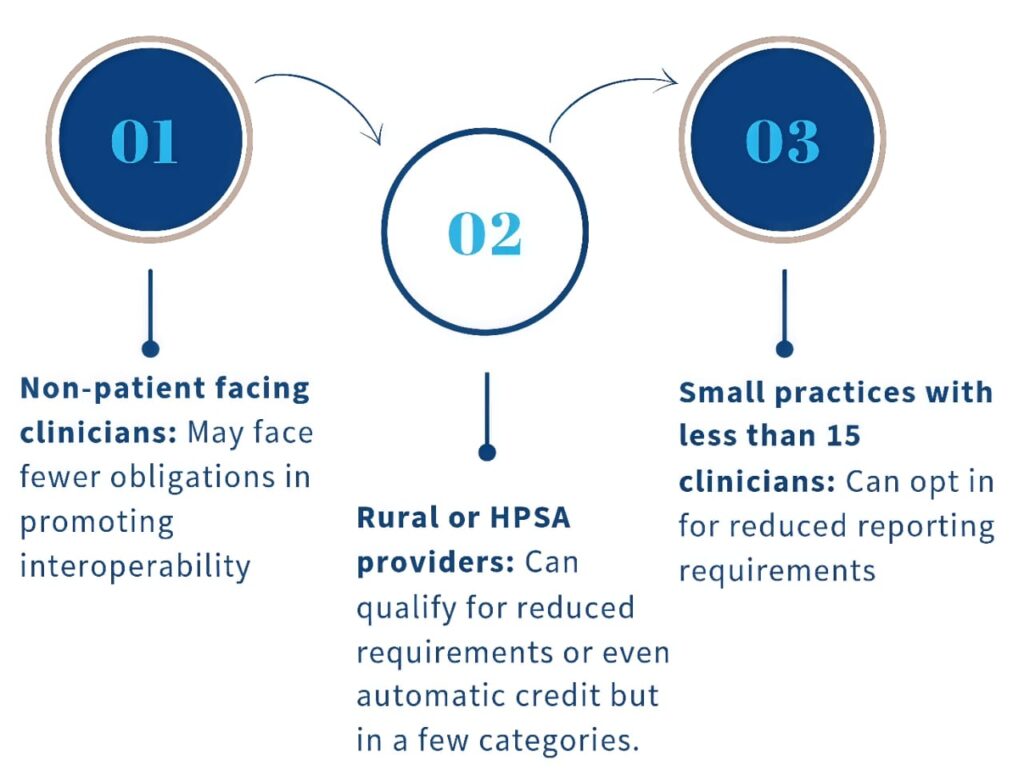
Special Considerations
Small practice: If a reported quality measure does not have national benchmarks, CMS will grant 6 bonus points even if they report on one quality measure. This will help protect them from being unfairly penalised. Rural and Health Professionals Shortage Areas: These practices may get extra scoring credit or special exemptions because of the challenges they face such as limited staff, fewer resources or even patient access issues.
Best Practices for Strong Quality Reporting
To perform well in MIPS 2025, you must plan everything ahead and follow these steps: Choose the right measures: Select measures that suit your specialty and patient demographics. Invest in technology to save time.
Bottom Line
CMS has made traditional MIPS quality reporting much easier and fairer than the last time. It’s now your turn to navigate it wisely by: Choosing right measure Tracking data all year Submitting on time to earn incentives
Why Choose A1 Healthcare?
MIPS quality reporting can be overwhelming, and A1 healthcare provides you an all-in-one package solution.
Our experts always stay updated with the latest CMS rules, so you don’t have to. We value your time so guide you through every detail till the end.

We don’t believe in the one-size-fits all approach. We take time to understand your specialty, team and patients to structure a plan that fits your needs.

Our team uses smart tools and EHR integration to make data collection and submission easier and faster.

With A1 healthcare, all of your queries will be taken care of. We consistently train your staff, provide valuable tips and share insights to help your practice improve every year.

APPOINTMENT
Book an Appointment Right Now
If you need any help with MIPS quality reporting 2025, reach out to us for free assessment.

Frequently Asked Questions
If your specialty measure set has less than 6 applicable measures, you need to report what’s available. For example, for ophthalmology if only 4 measures are relevant, you just need to report 4 and still can meet the requirements.
If you submit a measure below the 75% completion threshold, you are likely to earn only 1 point on the scale of 1-10 points.
No you cannot switch reporting methods. You must stick to one reporting method per category; however, you can use different methods across multiple categories.
Your performance is scored against national benchmarks based on 2023 data for 2025. If no benchmarks exist, you will only earn baseline points.
You can find all MIPS quality measures via the CMS-QPP website and quality measure inventory.

A1 Healthcare
Help Support
Services
Working Hours
- 8AM - 5PM
- Central Standard Time
- Monday - Friday
