(512) 377-1744
Introduction
The merit based incentive payment system or MIPS is an inevitable part of Medicare’s Quality Payment Program (QPP). This system is designed by CMS to reward all the healthcare providers who deliver high quality and cost efficient care to their patients. Similar to 2023, in 2024, the quality category remains the most important part of MIPS. CMS has made some updates that change how clinicians choose measures, report data and earn scores.

Updated Requirements of 2024
CMS set a total of 198 measures for the quality category for 2024 performance year. The purpose was to keep pace with updated medical standards.
New measures:
CMS finalized 11 new set of quality measures, which included:
- Ambulatory palliative care: To ensure patients feel understood (#495)
- Maternal Health: Tracking risks of cardiovascular diseases in pregnant and postpartum women (#496)
- Preventive care and wellness composite (#497)
- Mental Health risks: Safety planning for patients having suicidal risks (#504)
Other new measures focused on oncology, prevention and behavioural healthcare.

Removed Measures :
- 11 measures were completely removed because of topped out performance or they overlapped other important measures
- 3 measures were partially removed as they were kept for MIPS value pathways (MVPs)

Modified Measures:
A total of 59 measures were modified. These changes were made to:- Make instructions clearer than before
- Align with new healthcare guidelines
- Simplify and improve how measures were calculated
Quality Measures Updates for 2024
Measure Scoring in 2024:
In 2024, MIPS scoring was done on a 0-10 scale. However, the rules that apply to earn credits from these measures were changed as follows:
Performance score in 2024 used to depend on benchmarks, completion of data and minimum number of cases.
New measures get a head start:
- In first year — you get at least 7 points
- In second year — you get at least 5 points
Small practices with fewer number of providers always get 3 points even if data is not perfect.
Tips for Measures selection for MIPS 2024:
- Avoid capped measures as they offer only 7 points.
- Start with new measures as they start with a higher score so you get more points.
- Compare MIPS CQMs vs eCQMs and choose the version that scores the best and aligns with your data best.
Data Completion
This one was the most notable change in MIPS 2024. CMS increased the threshold for data completeness from 70% (in 2023) to 75%. All the providers must report on 75% of all eligible patients for each measure. The purpose was to make data more accurate and reliable because higher the threshold, greater the patients’ trust.
Performance Threshold and Data Scoring
As mentioned earlier, in 2024, you need 75 points for avoiding penalties. Otherwise: Less than 75% — Up to 9% penalties, Exactly 75% — Neutral Adjustment, More than 75% — Budget Neutral Incentive (exact number depends on the budget and final performance score)
Topped Out Measure Policy
Topped out measures are the quality measures where almost every clinician scores high. As there is no room for improvement in these measures to show so CMS capped them at score 7 points.
Bonus Points Policy
For 2024, bonus points policy has following requirements: Clinicians must report at least one outcome or high priority measure In case of reporting extra outcome or high priority measures, you get bonus points, Using a certified EHR system for reporting can help you earn extra credit too.
Public Reporting
MIPS scores affect both money and reputation. CMS publishes each clinician’s MIPS score online at Care Compare (formerly Physician Compare), Patients, employers, and payers have access to these scores while choosing doctors, A high score means more patients, higher trust and good quality care, A low score affects reputation and ultimately reduce patient choice
Reporting Timeline
There has been no change in reporting timeline since MIPS 2023. The performance year spans a 365 days period starting from 1st January 2024 to 31st December 2024. The submission period is the first quarter of 2025 and dates are already announced by CMS.
Benefits for Small Practices
Providers of small practices (15 or fewer members) are likely to receive following benefits: A 6 point bonus added to their total quality score Always get at least 3 points for a measure, even if data is incomplete Technical assistance support from CMS that make reporting easier
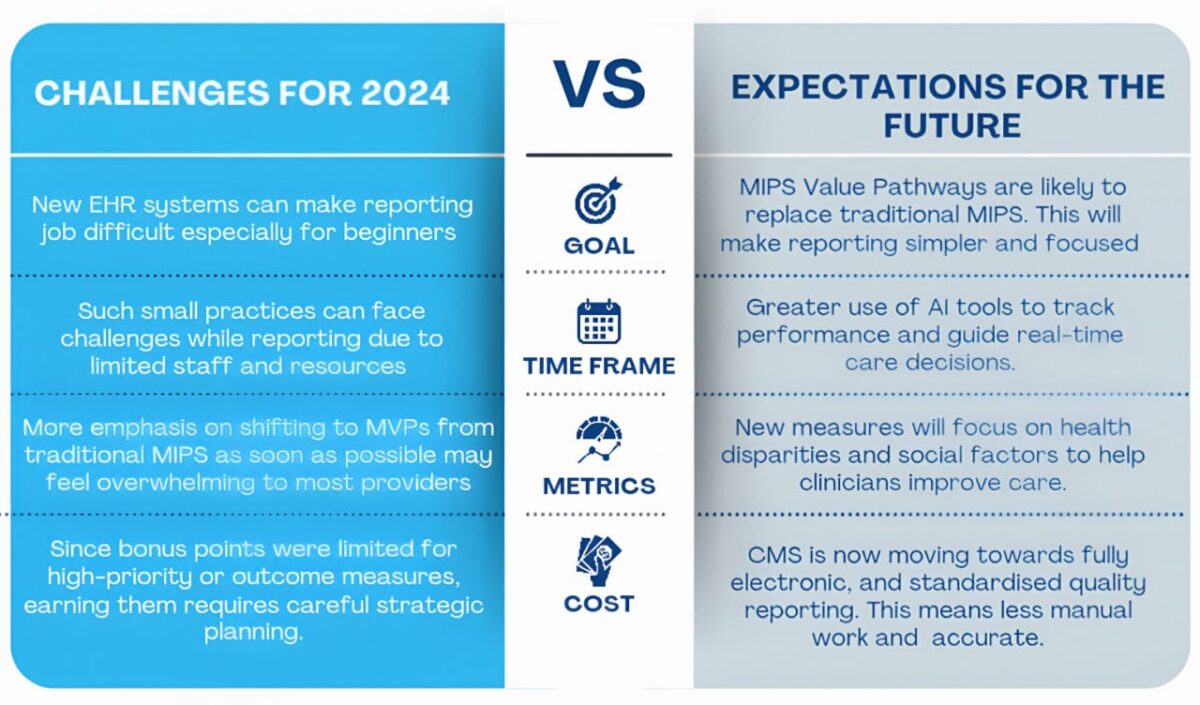
Expansion in MIPS Value Pathways
For 2024, following changes in MIPS value pathways or MVPs were made: 5 new MVPs were added, bringing the total to 16 available MVPs MVPs group quality, cost and improvement activities together for specific specialties to make reporting simpler and more relevant. The idea of replacing traditional MIPS with MVPs became stronger Considering these changes each provider needs to adjust to the new system and find out which MVP fits their practice the best.
Bottom Line:
Choose measures carefully, Track your practice’s performance throughout the year, Use high priority measures and earn bonuses, Prepare staff for MVPs and digital reporting in future, Stay updated for any changes.
Why Choose A1 Healthcare?
Due to significant changes in MIPS quality reporting, navigating in 2024 has become challenging. But A1 healthcare is here to make things simple for you.
At A1 healthcare, our experts know the rules, updates and pitfalls. Without confusing jargon or guesswork, we guide you through each step.

From choosing the right measures for your specialty to earning bonus points, we guide you through every step of the way. We don’t just report, we make your practice excel.

With modern EHR systems and automated tools we streamline the quality reporting for you. We ensure faster submissions with fewer errors.

Our team uses smart tools and EHR integration to make data collection and submission easier and faster.

Book a free consultation today!
Want to know more about MIPS quality reporting and how to transition smoothly to MVPs as soon as possible? Then contact us right now!


A1 Healthcare
Help Support
Services
Working Hours
- 8AM - 5PM
- Central Standard Time
- Monday - Friday
